
1/15 – Integral Design Leadership: Healthcare Design as Extraordinary Service: An Interview with Peter Jones
Lisa Norton
Lisa Norton


Lisa Norton

Peter Jones
Peter Jones is Associate Professor at Toronto’s OCAD University (Ontario College of Art and Design), an author and consultant in the emerging field of systemic design, and runs the innovation research firm Redesign Network. Peter spends his time balancing between teaching in the Strategic Foresight and Innovation graduate program in OCADU’s faculty of Design, pursuing collaborative research toward the redesign of social systems, and continues to redesign information services for medical and scientific clients.
Leveraging systems thinking, human-centered design, and information architecture, his Redesign Network serves the emergence of healthcare service systems capable of taking better care of human beings. By developing schemas for more comprehensive understanding of systemic conditions, Peter Jones is defining new intersections and innovation spaces in healthcare and information-intensive services. In the following interview, Dr. Jones shares first-person reflections and insights on patterns in organizational leadership and influence, as well as his hopes and concerns for the future of healthcare systems design.
As a hybrid of the techno centric and the vulnerability human, healthcare is a mega-system in the process of not just reforming but radically transforming. Peter Jones’ 2013 book, Design for Care: Innovating Healthcare Experience (2013, Rosenfeld Media) offers a leading edge, grounded overview of the challenges that this changing meta-system currently faces, and the obstacles to transformative change. Bridging the worlds of healthcare, clinical administration and design practice, Design for Care is theoretically grounded in both dynamic systems science and human centered design. With case studies developed by the Redesign Network, Design for Care is a rich compendium of key issues and innovative practices in research-driven engagements of whole systems design at touchpoints throughout the extended healthcare system.
In the developed world, every citizen is impacted on several levels by their proximity to or distance from, care services and health support. Design for Care reframes the objectified “patient” and “user” categories as health seekers. By reframing the patient role as health seeker and differentiating health seeking, (understood as ongoing and continuous throughout life) from information seeking, Design for Care makes space for a diverse range of individuals with multiple intentions. “These are patients receiving care for complex co-occurring illnesses, people improving their sleeping patterns, individuals struggling with the care needs of their family members. In nearly all cases, we have something in common – we are all seeking to improve health toward a felt homeostatic balance, the experience of a recognized sense of ‘normal’.” (Jones)
“Users” in the language of service design and “patients” in the language of healthcare, by holding the Other at arm’s length, confer professional neutrality yet inhibit our ability to empathize with the dilemmas of everyday encounters with health and disease. By enriching the meanings of health seeking, alternate scenarios, choices and possibilities can be envisioned.
“My strategies are related to changing the way we view and work with the “person” as a health seeker and not defined and limited to the role of patient. The reframing of the “center” of healthcare itself affords a new role for design that it hasn’t been able to play.” (Jones)
This Health Seeking Patient Journey infographic from Design for Care demonstrates how the health seeking frame, in blurring the boundary between actors inside and outside of the system, makes transparent complex roles and interdependencies. Language reframing is a designed intervention that actually creates spaces for more diverse lived behaviors that, over time, can translate into new and better practices and norms.
LN: The 2013 publication of Design for Care was perfectly timed with the national conversation (in the U.S.) about health care reform. I recently read Reinventing Organizations by Frederic Laloux, and I would be curious to know if you have studied the growth of the self-organized Buurtzorg neighborhood nursing organization so vividly profiled in Laloux’s book.
PJ: I am familiar with the Buurtzorg project from the Reinventing Organizations. I’m really very familiar with the previous waves of organizational reinvention in the US primarily, which occur about once a decade, almost like a business cycle. We seem to forget the learning from the profound leadership examples that have come (and often, sadly, gone) such as:
- Farming cooperative movements in the 1970’s and the mutualism of that era
- Radical high-tech firms of the mid-1980’s (Apple and Rolm were much different then) treated their employees as participants in an exciting adventure, along with the barefoot ethos, Friday beer blasts, rock bands in the terraces, etc.
- The mid-1990’s “soul of work” wave inspired by authors like Matthew Fox Margaret Wheatley, and David Whyte. Two of my doctoral mentors, Barry Heermann and Alex Pattakos were leading programs in the innovation of the meaning of work, and I’ve used their practices (Team Spirit and Seeds of Innovation) over the years.
I had real hopes for the 1999 manifesto from Malone, Orlikowski and the MIT Sloan School on inventing organizations for the 21st Century, to accord with our envisioned future and values. As this was right before the dotcom bust, it seemed the energy for change was washed out of the culture, and within two years we had Enron instead of Utopia. Significant “change” more often occurs in unwanted directions, and as a result of external forces, and even if events are foreseeable, the black swans are in the aftershocks. We thought Enron would be an opening for the ethical corporation, but just the opposite happened in many ways across the North American culture.
I had briefly worked for one such radical organization, Origin, founded by Dutch hippie Eckart Wintzen and organized around his learning from personal experience in researching indigenous cultures. Origin grew by self-organizing around cells of 50, as he discovered from tribal villages, where every individual can know every other personally, collaboration is a given, serving customers directly and maintaining a nearly flat hierarchy. I think these new movements give us hope, and examples of possible ways of rethinking the organization.
There are few truly flat organizations. The “hierarchy vs. network” theme is archetypal, but structure is not a solution. Networks are not flat by any means; they are lumpy and energized by power bases. Many hierarchies allow their departments to behave as if flat. Rather than characterizing by dichotomies, we might consider every system as a mix of structures, often shifting, but in slow motion. Large product companies often have vertical market segments and product lines that require separate teams and external networks, such as the large firm in We Tried to Warn You. And they were able to “learn lateral” when necessary, even in a traditional managed hierarchy.
Buurtzorg is in long term care, which enjoys a fairly stable care model that isn’t driven by turnover, clinical workflows, and the need for constant specialty interventions. Acute care hospitals are highly differentiated and require specialists across a general administrative infrastructure, and incorporate sequential, iterative and customized care. Long-term care is continuous and sequential, it’s not a complicated system. But I can see an autopoetic, self-organizing model working with the new Accountable Care Organizations (ACOs) now growing in the US, as these are often spun off from existing practices or medical centers, with determined clinical teams focusing on a local geography to provide primary or specialized care for all people in a region. ACO’s can be self-organizing and therefore dynamically created, staffed with a more diverse group of dedicated clinical professionals with an understanding of local patient needs, and then constituted within the provider ecosystem of a local region. They are much smaller than traditional medical centers, but can provide a core set of services, and compete for reimbursement effectively with low overhead and high focused quality. All kinds of new care models – sequential (primary), iterative (complex), and continuous, coordinated care services can be designed to fit the population and common needs of a region
LN: I’m curious to know if and how you see your strategies relating to or having been informed by, your personal experiences.
PJ: In terms of systemic design within organizations I’ve advocated (in both these books) a planned combination of top-down and bottom-up strategies of soft system design. My approach connects front-line projects with broad organizational and community goals. Through structured dialogue and creative workshops, we can help stakeholders in management and in patient-facing services to discover a shared framing of goals, boundaries, and roles to align their projects toward preferred system outcomes.
Healthcare practices are very resilient, they are trained and standardized so that many clinicians can be interchangeable and perform well under a range of conditions. Changing clinical practices, workflow or procedures requires strong evidence and a clear argument, retraining and evaluation. It’s the same thing when introducing a new EMR or IT system. Healthcare organizations are designed in a sense to resist change; they hold strong norms of practice due to the constant demand to serve their communities. Therefore when consultants (and designers) want to promote innovation and change and they don’t live and work inside healthcare – hospitals or practices – their proposals will likely fail. We are not all on the same team. Clinicians have a primary duty as caregivers – what is our duty of care to the caregivers? Perhaps as designers we can see possibilities those working in the domain cannot, but that doesn’t give a mandate for change from the outside.
Healthcare is risk-averse by design. It is (in Jane Jacobs’ terms) a guardian moral system, as opposed to a system of commerce or trade. Most consultants, designers and IT people come from companies with a commercial moral system, and their operating values may be inherently at odds. Is it ethical for “us” to advocate they act like traders? Technology interventions can have the effect of embedding a foreign values system, and as embedded, received without consensus. Jacob’s Systems of Survival shows why healthcare and other public services fit the guardian model; as with the military, healthcare is hierarchical and formal by the nature of the strong governance required in public systems..
And in my view, norms and values are not amenable subjects for direct design intervention and research. The more you research their function, the more they recede as a “design problem” and the more of a learning orientation seems needed. Values change from one’s learning and in relationship with others, not from a CEO’s change program or because we’ve created clever reflective feedback from an app. Design programs that believe they are addressing individual values change (or even so-called design for behavior change) risk imposing one’s own values and preferences.
Norms change with culture, and have to follow a natural cycle of adaptation within any organization. Chris Argyris cautioned about the difficulty of organizational learning, with the prevalence of typical “Model I” defensive behaviors, which apply to the adoption of new values and habits. People who are invested in an organization will raise defenses when change programs are introduced, and will claim to support the new behavioral regime (espoused values) while continuing to act upon embedded and historical values in use.
These days there are significant and increasing risks to healthy participation in healthcare organizations. Institutions and even practices are becoming highly-politicized due to increasing government austerity (“how our money is spent”) and political polarization (“whose health values are valorized.”). Transformational change programs espoused and imposed by management typically fail, often quickly, while work at the front lines of care is constantly intensified, manipulated by management, scheduling, and normal hierarchy. And while many health system business models are similar and clinical work follows well-known standard routines, every organization has its own strategy, unique culture and sense of place and belonging. Cultural change and clinical service change are not plug-and-play change operations – as I show in We Tried To Warn You, a “lateral” approach across peer-level functions facilitates robust, enduring organizational change. Following knowledge management theory, such a socialization model (from tacit to explicit learning) establishes resilient new functions based on small-group learning and not top-down “corporate retraining” programs.
LN: Would you elaborate on your first hand experiences facilitating large-scale, intra-and inter-sector system change in the context of your career?
PJ: The Redesign Network is a partnership organized around a continuing professional network, connecting top independent designers and researchers from Toronto and the US to client and research projects. Between the major universities in Toronto, the innovation community, and the OCADU Strategic Foresight program, we sustain continuity with a wide range of experienced, transdisciplinary research and design colleagues that can convene an amazing team when needed for the most interesting and complex challenges.
The doctorate studied embedded values in innovation practices within large software organizations, an activity theory approach to the structure of values systems within disciplinary groups (commonly known as stovepipes), the values of organizational power, and the systemic effects on impeding innovation. This research led to the action case study of the huge product failure of one firm, as told in the 2008 book We Tried to Warn You. Subtitled Innovations in Leadership for the Learning Organization, I discuss a management innovation that helped this company recover their market. My philosophy is to co-create an indigenous, resilient capacity based on existing talent within an organization, not to establish UX skills as exotic and externalized. Our approach was to socialize UX practices we developed for the must-win project, and with this visibility we then shared methods and artifacts across the company’s projects after they could see the team was achieving well, and not trying to compete for resources. In parallel, we were guided by senior management to merge with their product strategy following on several months of significant lateral development. This is institutionalization by bottom-up practice development, rather than department-building and training. There was no central user experience group – Redesign Network worked with the staff with the “best available” competencies and we learned in the field and through smart prototyping based on insights from observations of work in context.
In my experience, other creative competencies can be established within organizations, in a developmental way, not as a direct “culture change” initiative. Cultures change when internal practices reflect new values within ways of working. These practices, habits really, become communicated and valued across departments and enable significant improvements in complex work processes. I don’t believe that my role as a systems designer is to change culture however, it’s a designerly arrogance to believe we can change cultures as outsiders. We haven’t personally done that work in our own organizations, and even when I have, it was in an insider’s role of peer-led stewardship, not as a hired consultant. So how can we pretend our process design is the answer to complex sociotechnical work challenges? The best we can do is to facilitate dialogues and help internal teams design strategies for near and longer term transformations. My guides to these practices include systems thinkers like Christakis and Warfield (dialogic design) and Fernando Flores (“history making”), organizational theorists like Daniel Robey and Stuart Hart, social scientists Latour and Orlikowski, and the design methods and theory of (OSU’s) Liz Sanders and (IIT’s) Charles Owen. These are all contributors to systemic design in organizations requiring a rigorous, broadly-inclusive reach of stakeholders and relationships. But aiding these design dialogues is not to be confounded with leading cultural change, or designing organizational culture. That’s the proper role of enlightened leaders, both “senior” and emergent leaders, who have solidarity and empathy for the everyday concerns of the complex social system to which they are committed.
LN: From a macro trends perspective, would you discuss the key challenges and opportunities you are seeing and sensing coming at the intersections of design, health, and information?
PJ: This is a really large question, worthy of a whole interview. Let me frame a few of the possible trends that may conflict and resolve in interesting ways. I like to trace the difference in trends viewed from the go-go tech sector, supercharged by apparently inexhaustible Silicon Valley investment, and the trends seen from the clinical world, which has people to take care of and lives to save. In some ways these worlds couldn’t be more different – the divergence of culture and meaning between tech solutionism and the cultures of care. The gold rush into healthcare IT in the last five years has been astonishing – and yet changes to clinical practice and medical education are not driven by these value propositions
I expect to see massive consolidation after the startup boom realizes that financial returns are hard to recover in healthcare. The big EMR providers have the infrastructure locked up due to their cashing in on the HITECH Act.
Consider the diagram I call Health 3.0 (attached) that’s in Design for Care, which shows the core resources adopted in everyday clinical workflow over the last 5 years or so. While VCs and incubators might see these as a competitive field to be “disrupted,” I take the opposite view. These are all reasonably effective, dedicated, evaluated resources selected by healthcare institutions for long-term performance in the management of care. Doctors (especially) and others do not want to learn your app or discover new products – they have trouble enough remembering more than one password and managing the interfaces of critical EMR and patient data services. The business idea of disruption has little place here, there’s not much better a new entrant can do that would sway the installed base in many cases.
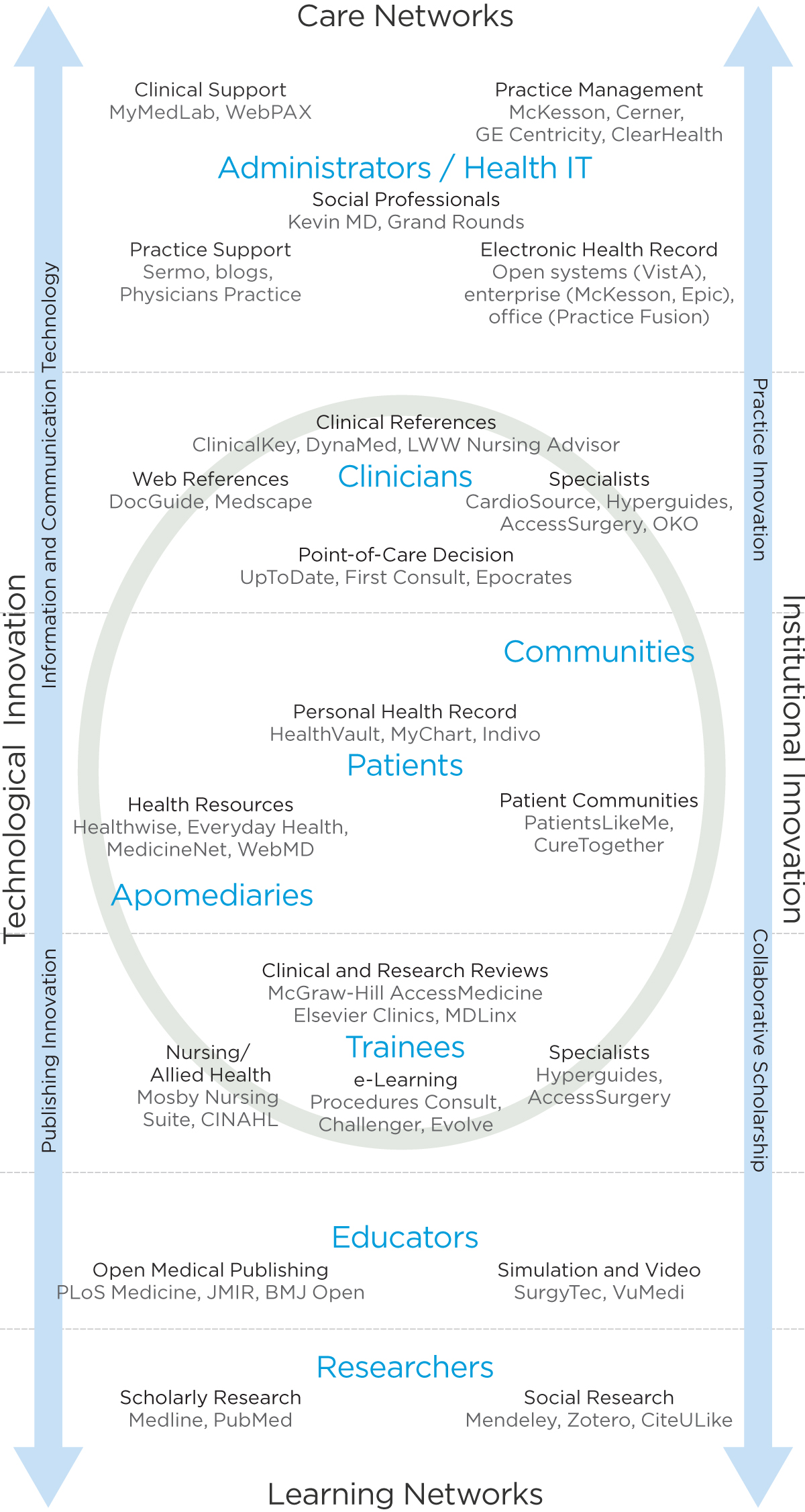
Health 3.0. Credit: Peter Jones, Design for Care: Innovating Healthcare Experience. Rosenfeld Media, 2013.
Consider one of my specializations, new media translation of evidence for medical care, for example. We might know exactly how to design a better user experience than UptoDate, but its viable market will be less than 5%. Healthcare practice is a field that’s defined by dedicated professional work, where skilled practitioners will train on a product maybe once, and rely on trusted vendors and quality information sources for practice decisions for a very long time. Interface changes are upsetting, and they don’t save much time. This is a content problem, and unless you’re a publisher of content, it’s not one solved by business model disruption. There are some free products in these spaces, and they are generally found unprofessional (or they aren’t fully featured).
Look at every other resource on this diagram – from what I call Care Networks to Learning Network, the range of workflows in practice. Very few are moved by upstarts – certainly not the major platforms for practice management and EHR systems. Even patient communities have not expanded like once thought. What counts is alignment to workflow, and if you do that, your interface will probably be close enough. And it goes without saying that the mobile experience is going to match the content and model of the parent platform in most cases, as no clinician wants to learn a separate interface for essentially the same workflow function.
I’m not sure how long this ecosystem will progress like this, and I have to say when I wrote the book and by 2013 I held back from making these claims. I was waiting to see whether some of these functions would be displaced, and now I’m more convinced that consolidation will happen around the strongest workflow providers. It’s an entirely different approach to design than Silicon Valley outsiders would promote in their disruption narrative.
LN: For design educators and emerging designers, Design for Care articulates the critical niches for design attention and contribution in the coming decade, as well as the capacities that emerging designers will require. What emergent trends and/or key challenges for medical or design education and/or practice are consolidating for you even since the publication of Design for Care?
PJ: I see two emerging thrusts in design for systemic change and sets of questions they suggest. One relates to clinical organizational change: How can we expand the functions of care within clinical organizations to enhance the design of service and the experience of care? How might design move from IT and other non-clinical services to the front lines? The other to health systems level: How can we design to engage and promote extraordinary care in our societies? How can we help clinicians move healthcare innovation from process improvement into a realm of “extraordinary service?”
LN: As a fellow design educator, I am inspired by your reframing of design agency as extraordinary service. It’s a powerful way of apprehending and communicating the untapped potential of design. As a design researcher, consultant and educator, you have cultivated a rich “T-shaped” capacities profile having theoretical grounding in dynamic systems thinking and human centered design, coupled with experience in applied design thinking and services design. I would imagine this unique combination of breadth and depth aids you in being with and inquiring into the kinds of complexity and volatility that characterize the multi-systemic state of healthcare provision today. How can design pedagogy better meet the challenges that the future will demand? What are the key skills and competencies that you attempt to instill in your students at OCAD?
PJ: The MDes in Strategic Foresight and Innovation was started in 2009, and is OCAD University’s most popular graduate degree now. It remains the only program of its kind in Canada and the US, as some with similar orientations have very different core courses. SFI is a unique mix of futures, design, and business practice thinking skills within a foundation of systems and visual thinking. Most faculty blend at least 3 meta-disciplines together. My background in design, research methods and systems for example, is underpinned by practical business experience and years of close collaboration with visual experts. We’re more H-shaped people than T’s, and our students are also demonstrating strong skills in two or more dimensions, with a transdisciplinary bar to connect them (the “H”).
Our approach to innovation instills a human-centered, systemic orientation to socially-responsive futures and applications. While we teach foresight methods and systems research for business, policy and social sectors, we encourage a long view toward systemic change. The kinds of complex social systems and Rittel-level wicked problems we work with have been with us in language and problem space since the 1960’s. They don’t budge by mere nudge, and certainly design labs and critique are insufficient to shift paradigms. Our grad students gain credibility as they land within sectors responsible for these longer-timeframe domains. Many of our students come from or are interested in complex healthcare, sustainability, urban ecosystems, and the many social sectors. We started off in 2008 identifying our program with social innovation, to distinguish our goals from business innovation, as we’re not an MBA. However, as social innovation started to trend toward micro startups and grassroots initiatives, we pivoted away from that understanding, since we’re in a long-haul kind of business. Startups are fine, but real systemic level work requires a strong network of relationships and resources over years. We’re finding a lot of our students connecting well in large institutions, perhaps surprisingly, but that’s who hires foresight and systemic design. The Government of Alberta has a very progressive internal consultancy that’s hired a number of our graduates as Systemic Designers (that’s their title.)
Our partnership with AHO has led to the symposium series, Relating Systems Thinking to Design, which enters its fourth annual turn in Canada at the Banff Centre this August. RSD started as a kind of regional, convivial workshop and paper share, and by last year has grown to attract the best speakers, students and practitioners in the interdiscipline we call systemic design. We were honored to host Dr. Ranulph Glanville’s final lecture before he passed away last December, as well as keynote talks last year by John Thackara and our own co-founder Harold Nelson. These talks, papers and presentations are available at systemic-design.net.
LN: I’d like to understand how you see your strategies relating to and having been informed by your personal experiences. What influences prepared you, as a designer and as a human being, to think creatively on the systems level and to hold organizational macro systems in dialogue and inquiry.
PJ: One of the most critical capabilities of a systems thinker is the ability to articulate boundaries, purposes and conditions expressed within and between boundaries. I’ve never accepted imposed boundaries very well; so perhaps find it very natural to hybridize knowledge and practices across fields as we’ve done in the SFI program, the RSD conference, and my books and publications. I’ve been in the leading practices of human-centered design since the 1980’s, working with IBM on their PC platform usability even before my human factors Masters degree. Later I consulted with AT&T and learned expert systems and knowledge engineering with a human factors group in Cincinnati linked to Bell Labs. When I finished my Master’s in 1991, the CEO of my former employer donated $1M to my school, the University of Dayton, to build a state of the art usability lab based on a model I proposed while an employee. My original plan called for about $25K, but was rejected by corporate cutbacks and was shelved. The CEO recognized this as a leadership opportunity, an amazing contribution. So one of my key learning moments was “you never know when your idea may come back for a bigger win.”
I worked as the first (or the only human factors / interface designer) at several places over the years, establishing good practices. At the systems company TASC I designed software and systems for the incoming Windows era in business and information systems. We failed early with a tool that Microsoft later built (and failed themselves), our TRIAN interactive office metaphor for management preceded Microsoft’s office assistant “Bob” by two years, and we knew what happened with Bob. I started designing web resources in 1994, and led the design for Elsevier’s ScienceDirect in 1996, as well as a number of the LexisNexis services on the web.
My early attraction to psychology, in high school, was in hopes of expanding the dimensions of human experience, and early on I was influenced by the radical psychologies of Tavistock and RD Laing, Eastern contemplative practices for spiritual awareness, and the intrapersonal depth psychology of Jung and later, Hillman. I trained early in learning these schools of thought and have been fortunate to have several influential teachers as mentors during college and young adulthood. I think we have lost these rites of passage now, and I’m trying to bring back cultures of cooperative learning though dialogue – but its not a substitute for the personal journey of learning from an elder’s tacit knowledge of a lifetime.
I find the disregard of our older population to be culturally bereft and quite sad. I notice that our North American culture now seems to expect the young to teach us – or save us from the world we made – as if there is something magical about their digital nativism that will better navigate the futures we live in now. It’s a kind of role abdication on our part that doesn’t bode well for generational learning. Young people haven’t gained the inner experience or learned through hardship as elders have, and don’t have a lifetime to teach from. We ought to be creating opportunities for purposeful contribution, not just volunteerism or the extension of one’s work life. I often fear for the lack of care in our society, the lack of an historical sense of place and purpose. When I’m in places like Norway, Japan, or parts of New England where my family is from, I see these connections across lifetimes and it restores a sense of hope.
LN: In closing, what achievements are you most proud of? And looking ahead, what is your crucial hope for the impact of your work in the coming years?
PJ: Making a real difference is something that’s earned through commitment, and it’s not guaranteed
References
Jacobs, Jane. Systems of Survival: A Dialogue on the Moral Foundations of Commerce and Politics. (1993, Random House)
Jones, Peter. Design for Care: Innovating Healthcare Experience (2013, Rosenfeld Media)
—, We Tried To Warn You: Innovations in Leadership for the Learning Organization (2008, Nimble Books LLC)
—, Team Design: A Practitioner’s Guide to Collaborative Innovation. (2002, Exlibris)
Laloux, Frederic. Reinventing Organizations: A Guide to Creating Organizations Inspired by the Next Stage in Human Consciousness (2014, Nelson Parker)
About the Participants
Peter Jones is associate professor in the Faculty of Design at Toronto’s OCAD University, teaching in the Strategic Foresight and Innovation MDes program. Dr. Jones founded Redesign Research in 2001, located in Toronto since 2010. A system and service designer, Peter has designed market-leading information services for healthcare, scientific, and business practices, and advises organizations on product/service design, innovation strategy and competency building. He founded the Design with Dialogue communities of practice designwithdialogue.com, a unique Toronto community learning and dialogue program. Dr. Jones has published over 15 peer-reviewed research articles and authored three books: Design for Care (2013, Rosenfeld Media), We Tried to Warn You (Nimble Books, 2008) and Team Design (McGraw-Hill, 1998). His research and trade articles can be found at designdialogues.com
Lisa Norton is a Professor in the Department of Architecture, Interior Architecture and Designed Objects at The School of the Art Institute of Chicago (SAIC). She holds the B.F.A. from Cleveland Institute of Art and the M.F.A. from the Cranbrook Academy of Art. The engaging power of crafted objects led her from fine art, via human interaction, into integral design. Norton teaches, writes, facilitates and consults to designers and organizations on curricular development and other values driven and designed change processes. designbeing.org.
